Robert A. Pierce IIFisheries and Wildlife State SpecialistSchool of Natural Resources
Emily FlinnResource ScientistMissouri Department of Conservation
White-tailed deer are susceptible to a variety of diseases, parasites and injuries. Although these conditions do not account for a large percentage of annual statewide deer mortality (typically less than 5 percent), in some situations disease or parasite outbreaks can impact a deer herd locally or regionally.
Infectious diseases of deer can be caused by pathogens that include some viruses, bacteria, parasites and abnormal proteins known as prions. In rare instances, these pathogens are the cause of disease epidemics that result in significant mortality in a local population. These outbreaks are most common in herds with high deer density, which can increase the spread of the disease.
Fortunately, disease and parasite outbreaks seldom impact the quality of venison or make it unsuitable for consumption.
This guide provides an overview of the diseases, parasites and injuries that can affect free-ranging white-tailed deer in Missouri.
Table of Contents
Diseases
Viral diseases
Hemorrhagic diseaseHemorrhagic disease is an infectious disease of white-tailed deer, with outbreaks occurring sporadically in Missouri. Hemorrhagic disease (HD) includes both epizootic hemorrhagic disease (EHD) and bluetongue (BTV) viruses. These diseases are very closely related and produce similar symptoms in deer.
Several species within the deer family are susceptible to the HD viruses, including white-tailed, mule and black-tailed deer. Domestic ruminants such as cattle and goats show no signs of illness or only mild signs when infected. In contrast, domestic sheep may develop severe illness when infected with the bluetongue virus.
HD is transmitted by biting midges of the genus Culicoides, thus disease outbreaks tend to occur from August to October, when midges are most abundant. The disease may go unnoticed in the wild because deer carcasses quickly decompose and are consumed by scavengers. Some infected deer may not show obvious symptoms; others may die in one to three days. Typical symptoms include fever; excessive salivation; swollen neck, tongue or eyelids; sloughed or interrupted growth of hooves; reduced activity; and emaciation (significant weight loss). Because sick deer are feverish, they are often found near water (Figure 1). However, in Missouri most deer that contract HD die quickly because they don’t have antibodies to fight the disease like deer in the southeast United States.
In Missouri, the severity and distribution of HD is highly variable. High-density deer herds may exhibit higher mortality rates due to increased contact between individuals, which allows infected midges to transfer from one deer to another. Incidence of the disease has ranged from a few scattered mild cases to dramatic outbreaks. Mortality rates during these outbreaks are usually below 20 percent; however, losses of up to 50 percent have been documented.
Not all infected deer will die from HD. The most common evidence that deer have survived the disease is from the sloughing, or cast and regrowth of hooves. These deer generally remain in good condition, and the hoof sloughing is simply a residual effect of the disease. In some cases, deer develop sores on their tongues, dental pads or insides of their cheeks. Their overall heath and condition will vary from excellent to poor depending on the severity of the secondary infection.
Humans are not at risk by handling or eating venison from an infected deer. Eating the meat of deer that have recovered from the disease poses no health hazard. However, deer may have developed secondary bacterial infections due to HD and thus, may not be suitable for consumption. If you find a dead deer and the cause of death is not apparent, report it to your local conservation agent (http://mdc.mo.gov/contact-us).
 Figure 1In Missouri, deer infected with hemorrhagic disease often die quickly and are found near water.
Figure 1In Missouri, deer infected with hemorrhagic disease often die quickly and are found near water.
Cutaneous fibromasCutaneous fibromas are wart-like growths caused by a virus that often infects deer through an open wound or insect bite. These growths can cover large portions of the body, but they are usually small, occur in single or multiple growths and range from a fraction of an inch to several inches in diameter. Fibromas are a more common occurrence in bucks because they are more likely to incur wounds while fighting and when rubbing antlers.
Although sometimes grotesque in appearance, fibromas generally do no harm to deer, unless they interfere with a deer’s sight or capability to eat. The virus does not infect other wild or domestic animals, or humans. Fibromas are confined to the skin and, therefore, are removed when the deer is processed for consumption. Thus, they do not affect or impact the quality of the venison.
Although sometimes grotesque in appearance, fibromas generally do no harm to deer, unless they interfere with a deer’s sight or capability to eat. The virus does not infect other wild or domestic animals, or humans. Fibromas are confined to the skin and, therefore, are removed when the deer is processed for consumption. Thus, they do not affect or impact the quality of the venison.
Bacterial diseases
Brain abscessesBrain abscesses are bacterial infections in the skull and brain. In white-tailed deer, brain abscesses most often occur in bucks (90 percent of cases) and are often seasonal, primarily due to the stages of antler development and fighting. During antler drop (casting) or severe fighting with other bucks, infections can develop on the skull near the pedicle, resulting in a brain abscess (Figure 2).
In the southeastern United States, brain abscesses are estimated to account for about 10 percent of natural mortality of mature bucks. Infection symptoms may include poor coordination, circling movements, blindness, lethargy (significant lack of energy) and emaciation.
The meat of a deer with a brain abscess is not suitable for human consumption.
 Figure 2Brain abscesses are more commonly found in mature bucks due to intense fighting. In this photo, green pus indicates the infected area of the brain.
Figure 2Brain abscesses are more commonly found in mature bucks due to intense fighting. In this photo, green pus indicates the infected area of the brain.
Lyme disease Lyme disease is caused by a bacterium (Borrelia burgdorferi) that is spread by certain tick species. The blacklegged tick (deer tick) is the primary species that transmits Lyme disease. Although deer and other wildlife can serve as a host for this tick species, they do not transmit the disease.
The life cycle of infection and the process of disease transmission begins during the spring, when tick eggs hatch into the larvae stage. During the summer, the larvae feed on several host species, including mice, squirrels, raccoons, rabbits and white-tailed deer. In the fall, the larvae mature into the nymph stage. The nymphs hibernate over winter. During the spring and summer, the nymphs are active and prefer to feed on mice, which serve as the reservoir (an immune host) for the disease.
No cases of humans contracting Lyme disease through the handling or consumption of venison have even been documented. Refer to the Ticks section below for precautions to take to minimize your exposure to ticks when handling deer.
Chronic wasting diseaseChronic wasting disease (CWD) belongs to a separate group of diseases known as transmissible spongiform encephalopathies (TSEs). TSEs cause brain degeneration in deer, elk and moose. The disease was first detected in a captive mule deer facility in Colorado in 1967 and since has been documented in free-ranging and captive white-tailed deer, elk and moose in several states.
The first deer that tested positive for CWD were found a few miles from a CWD-positive captive-hunting preserve in north-central Missouri in 2012. Since that year, CWD has been slowly spreading to other locations in Missouri and the number of deer testing positive have increased. Each year, the Missouri Department of Conservation tests a sample of the state’s deer population from hunter harvested deer for the disease. CWD testing has two main goals: detect the disease as early as possible in new locations and monitor changes in disease occurrence over time. Focusing testing on adult males increases the likelihood of finding CWD in new areas. Within CWD Management Zone counties (counties within 10-miles of CWD detections), a greater number of samples are collected, due mostly to “mandatory sampling” on opening weekend of fall firearms season. More detailed information on CWD surveillance and locations in the state that require mandatory sampling can be found on the Missouri Department of Conservation website.
The symptoms of CWD-infected deer include a change in the animal’s natural behavior, emaciation, excessive salivation, lethargy, stumbling and tremors. The disease is always fatal to the infected animal, but symptoms can take months or years to appear. Diagnosis can only be confirmed by laboratory examination of brain or lymph node tissue of an animal (Figure 3).
The movement and transportation of captive live animals, hunter-harvested deer or carcasses are the greatest risk factors for the spread of CWD into new areas. Natural movements of free-ranging deer can also contribute to the spread of the disease.
Once the disease is established, CWD spreads through animal-to-animal or soil-to-animal contact. Unfortunately, CWD can persist in the environment for a long time. Activities intended to concentrate deer to a location, such as feeding and placement of minerals or salt, are discouraged because direct and indirect contact at these locations can promote the transmission of the disease.
CWD tends to exhibit a clumped distribution on the landscape centered on the point of introduction. The targeted culling of deer near CWD-positive locations is one management strategy that may help limit the increase of CWD prevalence within a population. Additionally, minimizing the unnatural concentration of deer at feeding and mineral sites can reduce the risk of spreading CWD.
Chronic wasting disease is not seen as a human-health issue. The Missouri Department of Health and Senior Services and the Centers for Disease Control and Prevention (CDC) have determined there is no evidence CWD can infect people. According to the Missouri Department of Agriculture, there is no evidence that CWD can spread from an infected animal to domestic livestock, such as sheep or cattle. The Missouri Department of Conservation continues to sample deer for CWD. If you observe or harvest a sickly deer, please contact the Missouri Department of Conservation. You can learn more about CWD at http://mdc.mo.gov/CWD.
 Figure 3To test for CWD, the retropharyngeal lymph nodes, the obex of the brain or both are collected and sent for testing.
Figure 3To test for CWD, the retropharyngeal lymph nodes, the obex of the brain or both are collected and sent for testing.
Parasites
Nematodes
Arterial wormsArterial worms live in the arteries of white-tailed deer. Deer contract arterial worms when bitten by infected horseflies. Infections can result in food being impacted under the tongue causing facial swelling, with occasional tooth loss and jawbone degeneration (Figure 4). However, deer infected with a small number of worms will not exhibit symptoms. Arterial worms pose no threat to humans, and the venison of infected deer is safe for consumption.
Figure 4This area on the deer jawbone appears to be infected by an arterial worm.
LungwormsAs their name implies, lungworms infect the lungs. Only deer with severe lungworm infections exhibit symptoms, which include emaciation, respiratory distress (trouble breathing) and lethargy. Lungworm infections commonly occur in fawns in high deer density areas. The presence of this parasite provides additional motivation for maintaining deer population densities below an area’s biological carrying capacity. Lungworms pose no health threat to humans, and the venison of infected deer is safe for consumption.
Arthropods
TicksAbout 18 tick species have been reported to infect white-tailed deer. The three species most commonly found on deer in Missouri are the lone star, blacklegged (deer tick) and American dog ticks (Figure 5).
In most cases, deer infected with ticks do not show any symptoms, and tick infections rarely lead to death. However, deer with severe tick infections may experience irritated skin around the tick site, weight loss and secondary infections. Severe tick infections can also lead to poor body condition.
Ticks can also affect many other wildlife species, domestic livestock and humans. Humans are susceptible to several tickborne diseases, including Lyme disease and ehrlichiosis. When handling and processing infected deer, take these precautions to minimize your exposure to ticks:
- Hang the deer carcass for a day or two to allow the ticks to drop off.
- Wear latex gloves.
- Treat clothing with a tick repellent to decrease your exposure.
- Take a shower and check your body for ticks after being outdoors.
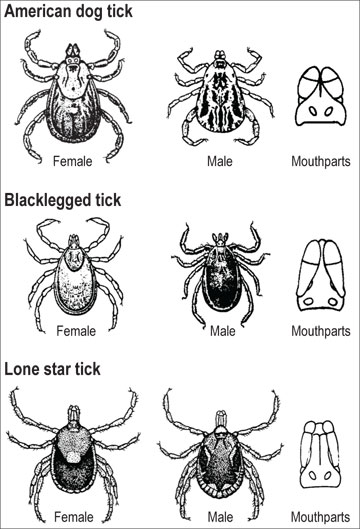 Figure 5The three ticks most commonly found on deer in Missouri are the American dog, blacklegged and lone star ticks.
Figure 5The three ticks most commonly found on deer in Missouri are the American dog, blacklegged and lone star ticks.
Mange (Demodectic)Demodectic mange of white-tailed deer is caused by the mange mite. Although most deer will not show symptoms of mange, those that do will exhibit hair loss and skin thickening with small pus-filled lesions. Mange is primarily spread through contact with an infected deer or its environment. However, mange does not cause a herd health issue and is not a concern for humans. Mange infections are limited to the skin, therefore the meat of an infected deer is safe for human consumption.
Nasal botsNasal bot flies (Cephenemyia spp.) are common parasites that infect the nasal passages of deer. They also infect squirrels and rabbits. These parasites are most often found by taxidermists while preparing heads for mounting, although hunters occasionally notice them.
Adult female flies deposit small larvae in the nostrils of deer. The larvae enter the nasal passages and pass through several stages of development and growth. They are liberated from the nostril when the deer sneezes. They then form a pupa and emerge as an adult fly.
Although quite large (up to 11/2 inches long) and unpleasant looking in the final stages of development, nasal bots cause little harm to deer and do not infect humans. They also do not affect the quality of venison.
Injuries
Deer that have suffered injuries are occasionally harvested by hunters. Injuries may result from hunter-inflicted wounds, deer-vehicle accidents or incidents with fences or farm equipment. Many of these injuries heal without complication, but occasionally they cause infections that cause dead tissue and pus in and around the wound. Although localized infections or abscesses caused by an injury do not pose a problem to overall deer health, they can pose a local meat-safety problem. If an abscess is discovered, it must be trimmed out. If it has been accidentally cut or removed and has leaked matter onto the surrounding tissue and meat, that meat is considered contaminated and must trimmed out as well.
Conclusion
Infections resulting from diseases and parasites typically result in only a small percentage of annual deer mortality. However, hunters and landowners should be familiar with the possible symptoms, and hunters that eat venison should be able to identify disease symptoms when field-dressing and processing deer. Contact the Missouri Department of Conservation if you see a deer with an apparent disease or that looks unhealthy.
Additional references
- Campbell, T. A., and K. C. VerCauteren. 2011. “Diseases and parasites” in Biology and management of white-tailed deer, ed. D.G. Hewitt, 219-249. Boca Raton, FL: CRC Press.
- Davidson, W. R., ed. 2006. Field manual of wildlife diseases in the southeastern United States, 3rd ed. Athens, GA: University of Georgia.
- Southeastern Cooperative Wildlife Disease Study. The University of Georgia College of Veterinary Medicine. https://vet.uga.edu/scwds







































![Air gun 101: The differences between .177 & .22 – Which jobs they do best ? [Infographic]](https://airgunmaniac.b-cdn.net/wp-content/uploads/2024/11/1773-150x150.jpeg)
